Subglottic stenosis information
The larynx or the voice box is at cross roads of the wind pipe and food pipe. The larynx consists of the vocal cords which allow vocalisation and also protect the lungs during feeding. The subglottis is located just below the vocal cords. The vocal cords represent the narrowest portion of an adult airway and the subglottis that of an infant airway.
Subglottic stenosis is narrowing of the subglottic airway. The narrowing can vary from minor (50% airway lumen obstruction) to a severe closure (100% airway lumen obstruction). Even minor degrees of narrowing can have disastrous consequences in a small infant airway as compared to a larger adult airway.
Causes
There could be many reasons which lead to narrowing of the subglottis. The causes are different in infants and adults. Generally, there are 3 possible causes: congenital, acquired and mixed.
In small babies, the narrowing occurs secondary to an existing congenital condition of the cricoid cartilage (cartilage of the subglottis). At birth, the cricoid can be small, elliptic or very thick. In all the 3 types, the subglottis is very narrow. Most acquired cases of subglottic stenosis occur in the first few months of life and can result from needing a breathing tube inserted into the airway (intubation), particularly when a baby is born prematurely or has other associated heart and lung conditions. In the mixed category, an intubation is added onto a pre existing cartilage deformity.
In adults, subglottic stenosis can occur following prolonged / repeated intubations (in intensive care units), tracheostomy, neck trauma, vehicular accident, strangulation and Wegener’s granulomatosis.
Patient presentations
It is very obvious that the main presentation of a patient with subglottic stenosis is breathing difficulty. The breathing is noisy, harsh (stridor) and the patient has shortness of breath, especially with increased activity. The voice can get abnormal with increasing airway narrowing. Very typically, a child gets fatigued when playing. An adult may find it difficult to climb increasing flights of stairs or get fatigued during exercise.
Severe narrowing of the airway will need examination of the entire airway and probably placement of a tracheostomy(artificial opening through the skin into the windpipe). The tracheostomy is placed below the narrowed section, thus bypassing the stenosis and allowing the patient to breathe. The actual treatment of the stenosis is then planned and various options will be discussed with the patient.
Diagnosis
It is imperative that the patient is examined by a specialist. Sometimes, recurrent episodes of respiratory infections (croup, bronchial asthma) can actually mimic an underlying airway stenosis. The parents and the treating physician should be aware and vigilant of this condition.
The history of the patient leads to the diagnosis. Confirmation of an airway stenosis is done by performing a procedure called transnasal flexible laryngoscopy and bronchoscopy. The endoscopy allows the doctor to look into the patient’s airway (nose, throat, back of the tongue, larynx, trachea and bronchi) using a small telescope and light.
Is it an emergency when diagnosed of a subglottic stenosis?
Absolutely. It is important for the treating physician to be aware of this condition because it takes a very short time for the condition to go from bad to worse, especially in very small babies. Emergency airway management in a known case of stenosis should be done only by an experienced team of doctors. Subglottic stenosis is graded from one to four starting from the mild to the most severe form of obstruction.
Remember, even a minor cold can cause the tissues of the larynx to swell (common in small children with small airways) and this can cause severe respiratory distress. This is very typical of a minor grade stenosis, when the patient has only mild symptoms.
Treatment
There are several factors that are considered while choosing the right surgical option. These depend on the severity and site of stenosis, length of the stenotic segment, and associated conditions such as: cardiopulmonary conditions, neurological status and associated comorbidites. All these play an important role in the final result.
Majority of children with severe comorbidites already have a tracheostomy. They could have a feeding tube passed into the stomach (PEG-percutaneous endoscopic gastrostomy) and may be delayed in their development. Multiple levels of airway stenosis and comorbidities complicate the final end result. All these will be discussed between the family and the treating doctors who will give a realistic idea of what to expect after the treatment.


We have treated a large number of complex airway stenosis with excellent results. Needless to say, the quality of life for the family after a child is decannulated (removal of the tracheostomy) cannot be imagined. The future outlook for such patients is very good if there are no associated comorbidites.
There are number of options for treating the patient with mild to severe subglottic stenosis. Operations include dilatation, laryngotracheal reconstruction, or cricotracheal resection. A congenital subglottic stenosis should never be dilated.
Voice outcome after airway stenosis surgery
One of the points that must be considered during the treatment for subglottic stenosis is the voice. Majority of patients should have a communicable voice after surgery, though it may not be completely normal. Voice gets better with time and speech therapy and could get close to normal. It must be remembered that, there is always a trade-off between the AIRWAY and the VOICE when performing surgical interventions on the subglottic airway. Priority is given to decannulation (removal of the tracheostomy canula) which changes the quality of life for the patient and avoids multiple problems associated with the tracheostomy.
To improve voice, various endoscopic procedures can be done once the tracheostomy is removed permanently.
Post operative period
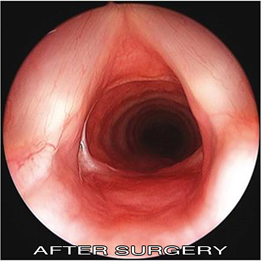
After surgery, the patients are closely followed up performing endoscopies at regular intervals (1, 3 months). During this period, the patients need to maintain a flexed position of the neck and avoid heavy activities and sports. Complete healing after a satisfactory intervention takes 3 months. Final endoscopy is done at 1 year following the airway reconstructive surgery.
When can we remove the tracheostomy definitively (decannulation)?
For patients staying outside Switzerland, a systematic plan of follow up is prepared taking into consideration the long distance of travel and individual country insurance policies.



