Researchers at EPFL and Lausanne University Hospital (CHUV), led by professors Grégoire Courtine and Jocelyne Bloch, have achieved a major milestone in the treatment of spinal cord injuries (SCI). By applying deep brain stimulation (DBS) to an unexpected region in the brain—the lateral hypothalamus (LH)—the team has improved the recovery of lower limb movements in two individuals with partial SCI, greatly improving their autonomy and well-being.
Wolfgang Jäger, a 54-year-old from Kappel, Austria, has been in a wheelchair since 2006 after a ski accident left him with a spinal cord injury. Participating in the clinical trial, he experienced firsthand how deep brain stimulation could restore his mobility and independence. “Last year on vacation, it was no problem to walk a couple of steps down and back to the sea using the stimulation,” Jäger shared, describing the newfound freedom DBS has given him. Beyond walking, the therapy has improved everyday tasks. “I can also reach things in my cupboards in the kitchen,” he added.
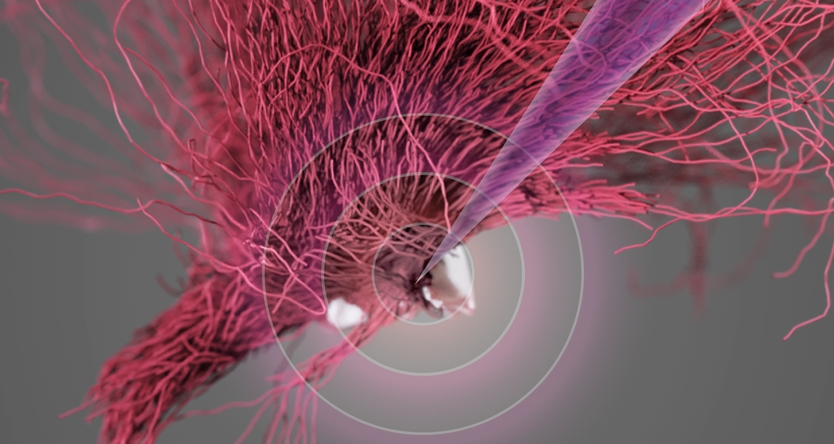
DBS is a well-established neurosurgical technique that involves implanting electrodes into specific brain regions to modulate neural activity. Traditionally, DBS has been used to treat movement disorders like Parkinson’s disease and essential tremor by targeting areas of the brain responsible for motor control. However, applying DBS to the lateral hypothalamus to treat partial paralysis is a novel approach. By focusing on the LH, the researchers at .Neurorestore tapped into an unexpected neural pathway that had not been considered before for motor recovery.
In the study published in Nature Medicine, not only did the DBS show immediate results to augment walking during rehabilitation, but patients also showed long-term improvement that persisted even when the stimulation was turned off. These findings suggest that the treatment promoted a reorganization of residual nerve fibers that contribute to sustained neurological improvements.
“This research demonstrates that the brain is needed to recover from paralysis. Surprisingly, the brain is not able to take full advantage of the neuronal projections that survive after a spinal cord injury. Here, we found how to tap into a small region of the brain that was not known to be involved in the production of walking in order to engage these residual connections and augment neurological recovery in people with spinal cord injury,” says Courtine, professor of neuroscience at EPFL, Lausanne University Hospital (CHUV) and UNIL and co-director of the .NeuroRestore center.
Fundamental neuroscience combined with neurosurgical precision
The success of this DBS therapy hinged on two complementary approaches: discoveries enabled by novel methodologies in animal studies and the translation of these discoveries into precise surgical techniques in humans. For the surgery, the researchers used detailed brain scans to guide the precise locations of the small electrodes into the brain, performed by Bloch at CHUV, while the patient was fully awake.
“Once the electrode was in place and we performed the stimulation, the first patient immediately said, ‘I feel my legs.’ When we increased the stimulation, she said, ‘I feel the urge to walk!’ This real-time feedback confirmed we had targeted the correct region, even if this region had never been associated with the control of the legs in humans. At this moment, I knew that we were witnessing an important discovery for the anatomical organization of brain functions,” says Bloch, neurosurgeon and professor at the Lausanne University Hospital (CHUV), UNIL and EPFL, and co-director of the .NeuroRestore centre.
The lateral hypothalamus’ role in walking recovery
The identification of the LH as a key player in motor recovery after paralysis is in itself an important scientific discovery, given that this region has traditionally only been associated with functions like arousal and feeding. This breakthrough emerged from the development of a novel multi-step methodology that began with whole-brain anatomical and functional mapping to establish the role of this region in walking, followed by experiments in preclinical models to establish the precise circuits involved in the recovery. Ultimately, these results led to clinical trials in human participants.
“It was fundamental research, through the creation of detailed brain-wide maps, that allowed us to identify the lateral hypothalamus in the recovery of walking. Without this foundational work, we would not have uncovered the unexpected role this region plays in walking recovery," says Jordan Squair, a lead author of the study.
The advanced imaging platform at the Wyss Center played a critical role in this research by providing high-resolution imaging capabilities that enabled the team to map the anatomical and functional activity of neurons across the brain, enabling the identification of the lateral hypothalamus.
Combining DBS with spinal implants for enhanced recovery
These remarkable results pave the way for new therapeutic applications to augment recovery from SCI. Future research will explore integrating DBS with other technologies, such as spinal implants that have already shown their potential in restoring movement after SCI. “Integrating our two approaches—brain and spinal stimulation—will offer a more comprehensive recovery strategy for patients with spinal cord injuries,” says Courtine.
Contacts for journalists
EPFL : presse(at)epfl.ch
Lausanne University Hospital (CHUV) : medias(at)chuv.ch
Pictures and video
Press kit for journalists
For medical information, please fill the form on .NeuroRestore